- Clinical audit comprises four key stages (Figure 1):
Preparation and planning
- This stage involves identifying an area where there may either be problems or where there are certain standards that need to be met. This then necessitates the setting of standards for the quality improvement project.
- These could be derived at a:
- Local level – i.e. hospital derived
- Regional level
- National level – i.e. from a specialist organisation (i.e. BOAST guidelines)
- These standards/guidelines should be evidence based and should be objective and be able to be measured. They should also reflect best practice in the chosen area and facilitate the ability to make changes.
- This stage should identify where and how data should be collected.
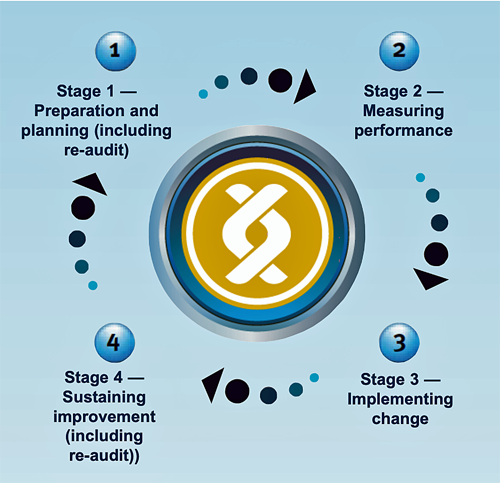
Figure 1. HQIP Clinical Audit Cycle
Measuring
- Measurement of clinical practice requires the auditor to have:
- A population to audit:
- This should be predefined with inclusion and exclusion criteria as appropriate and should be done over a specified time frame.
- A data collection tool, this can be either:
- As part of a standardised collection tool from a local/regional/national organisation.
- Devised by an auditor to look at specific quality measures.
- Once data are collected they must be analysed before implementing change.
Implementing change
- This requires comparison of current practice, as collected during stage 2 of the cycle (Measuring), with best practice and identifying areas where change needs to be made.
- Changes made to practice are often in line with the other key areas of clinical governance, these can include:
- Education and training
- Clinical effectiveness
- Risk management
- Staffing management
Sustaining improvement
- This requires maintenance of the changes to practice in line with best practice standards. Again, this necessitates adherence to the other key components of clinical governance.
- One of the fundamental parts of clinical audit and sustaining improvement is re-audit. It is often referred to as completing the cycle and entails repeating the stages of clinical audit to provide objective evidence that the improvement is sustained.