Introduction
- The isolated spine is an unstable structure. It has a critical buckling load of around 350 N, roughly the weight of head and upper torso. Yet the spine does not collapse, due to the stabilising role of the spinal muscles. Spinal ligaments are viscoelastic and loading rate sensitive. This allows effortless spinal movement in a physiological range but provides a very rigid structure against high loading.
- Vertebral bodies support the weight and gradually increase in bulk as we go down. They are made of a thick cortical shell filled with cancellous bone. The cancellous trabeculae are oriented in both vertical as well as transverse directions to resist multidirectional compression. The cancellous core carries around 55% of the load through a motion segment dropping to 35% with age and osteoporosis. Cancellous bone resists compressive load and cortical shell provides stiffness against torsional and bending load. This composite structure is best suited to keep weight at the minimum while resisting loads from different directions.
- Intervertebral discs are composed of a nucleus pulposus core enveloped by annulus fibres. Nucleus is mainly water (75–89%), type II collagen and proteoglycan. This allows the nucleus to act like a hydrostatic buffer during loading – redistributing load more uniformly and storing energy. Annulus has type I collagen. The fibres in annulus are arranged in bands at alternative 30° orientation to the end plate. Again the alternating arrangement of fibres allows annulus to resist loading from all directions. When loaded the disc acts as a thick walled pressure vessel
Spinal Stability (White & Panjabi) (1)
• Ability of spine to resist displacement under physiologic loading in order to protect the neural structures from damage and prevent deformity and pain
Denis 3 column theory (2)
- Denis described the three column concept to describe stability of spinal injury. The posterior column consists of the posterior ligamentous complex. The middle column includes the posterior longitudinal ligament, posterior annulus fibrosus, and posterior wall of the vertebral body. The anterior column consists of the anterior vertebral body, anterior annulus fibrosus, and anterior longitudinal ligament. An injury with two or more column involvement is unstable.
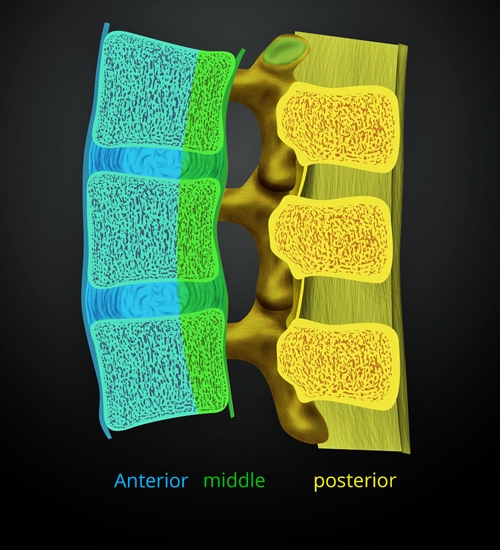
Figure 1. Denis three column theory
Motion Segment
- This is also called a functtional spinal unit or articular triad
- A spinal motion segment is two adjacent vertebrae,the intervertebral disc,facet joints and all intervening soft tissues(ligaments) but excludes muscle
- The functional spinal unit is the smallest physiological unit of the spine that exhibits biomechanical properties similar to that of the entire spine.
Spinal stability
Although a number of theories for spinal stability exist the model described by Panjabi has gained widespread use
Spinal stability is conferred by the interaction of 3 subsystems
1. Passive musculoskeletal system
2. Active musculoskeletal system
3. Neural system
The three subsystems work together to provide the overall stability of the spinal system
1. Passive musculoskeletal system
Includes vertebrae, intervertebral discs, facet Joints, ligaments, joint capsules
Vertebrae
- Vertebral bodies support the weight and gradually increase in bulk as we go down. They are made of a thick cortical shell filled with cancellous bone.
- The cancellous trabeculae are oriented in both vertical as well as transverse directions to resist multi-directional compression.
- Cancellous bone resists compressive load and cortical shell provides stiffness against torsional and bending load.
- This composite structure is best suited to keep weight at the minimum while resisting loads from different directions
- S shape in sagittal plane allows body weight to be away from the central axis of rotation, which aids balance and gait
- Axis of rotation goes through posterior part of vertebral body
Intervertebral discs
- Intervertebral discs are composed of a nucleus pulposus core enveloped by annulus fibres.
- Nucleus is mainly water, with type II collagen. This allows the nucleus to act like a hydrostatic buffer during loading- redistributing load more uniformly and storing energy.
- Annulus has type I collagen. The fibres in annulus are arranged in bands at alternative 30º orientation to the end plate. Again the alternating arrangement of fibres allows annulus to resist loading from all directions.
Facet joints
- The facet joints are part of the posterior column. They are load bearing and could carry 1/3rd of total spinal load. Spinal movement in each segment is guided by the orientation of the facet joints.
- Vertebrae have six degrees of freedom of movement. All types of cervical motions are allowed, thoracic segment allows flexion/extension, lateral flexion and rotation; lumbar motions are flexion/extension, lateral flexion but hardly any rotation.
- They determine type of movement possible between a vertebrae
- Caudally become more vertical in the sagittal and coronal plane 45-60-90 degrees and 0-20-45 degrees respectivel
- Cervical spine is resistant to translation but susceptible to flexion/extension because of obliquity of facet joints
- Lumbar spine is much more resistant to flexion/extension
- Thoracic spine has extra stability because of rib cage
- During quiet standing the centre of gravity goes anterior to the vertebral body, the spine is subject to a forward bending moment so the spinal muscles are constantly active. Any forward bending would increase the moment arm and increase load
Spinal Ligaments
• Flavum
o High density of elastin, which prevents it buckling inward
o When degenerate these properties change
o Facet overriding allows flavum to buckle in stenosis
• PLL & ALL
o Strong resistors of flexion and extension
• Others – inter transverse and interspinous ligaments
2. Active musculoskeletal system
Consists of the spinal musculature
Extensor muscles, abdominal muscles, intercostals, lower trunk muscles
Extensors are in 3 layers
- Deep
- Interspinalis, intertransversalis
- Intermediate
- Between deep layer and transverse processes
- Multifidus, Semispinalis
- Superficial (erector spinae)
- Longissmus, Spinalis, Iliocostalis, Splenius
3.Neural Subset
- Activates and controls muscle force generation
- Involves proprioception which is essential as the spine is constantly changing positions and loading
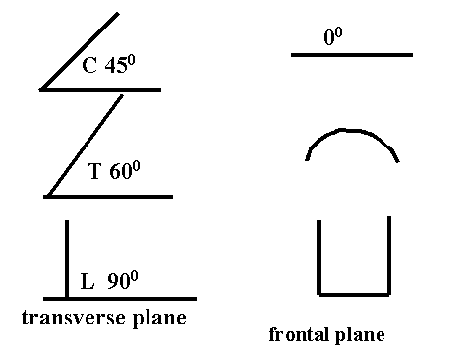
Figure 2. Facet joint orientation
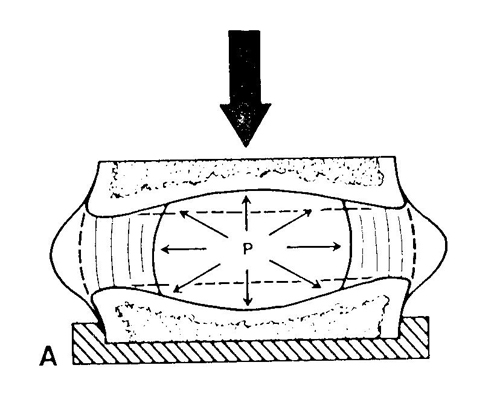
Figure 3. IVD with compression
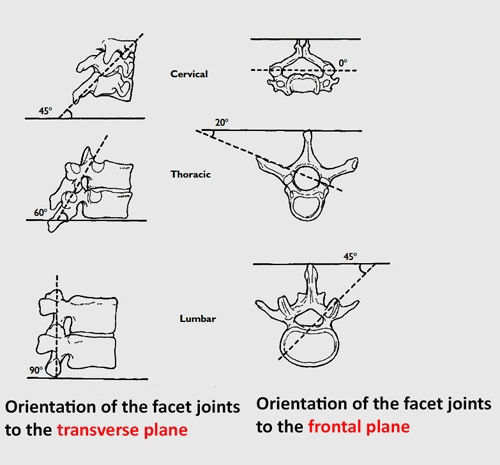
Figure 4. Face joint orientation
.jpg)
Figure 5 (a). Rotation mid thoracic facet joints
.jpg)
Figure 5(b). Rotation thoracolumbar junction facet joints
Incorporation of systems in spinal stability
Spinal range of motion has a neutral zone and an elastic zone
Neutral zone
- Initial zone of high flexibility where the active and neural systems predominate to give proprioceptive feedback controlling motion
- The motion region of the joint which functions independently of the osseoligamentous complex with a relatively small load producing a large displacement
Elastic zone
Towards the end range of motion where the passive system predominates to limit movement and prevent damage to the neural structures (stability)
Spinal Disease or Injury
In degenerative disease or burst fracture:
- The size of the neutral zone is increased
- It is increased to greater than the total physiologic motion of the spine
- The stabilizing systems do not reach the stiffening phase of the force displacement curve
- This means there is a much wider zone of movement where neurologic injury may occur
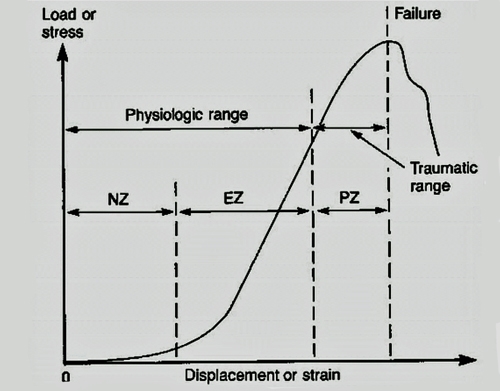
Figure 6. The load-displacement curve of the spine is generally nonlinear. At small loads, there is relatively large displacement; at larger loads, there is relatively less displacement. This load-displacement curve may be divided into physiologic and traumatic ranges. The physiologic ROM may be further divided into two parts(1)NZ, which is the displacement beyond the neutral position due to application of a small force,(2) EZ, more load is required per unit displacement. The traumatic range is defined by the PZ; it is the displacement beyond the EZ to failure.