Case based Discussion Periprosthetic knee fracture
A 72-year-old lady presents to ED following a fall on pavement. She complains of pain around the right knee arthroplasty performed 7 years previously. She did not have any knee discomfort or symptoms prior to the fall. She is independent with activities; medical comorbidities include Type 2 Diabetes Mellitus and ischemic heart disease.Her radiographs are shown below (Figure 1)
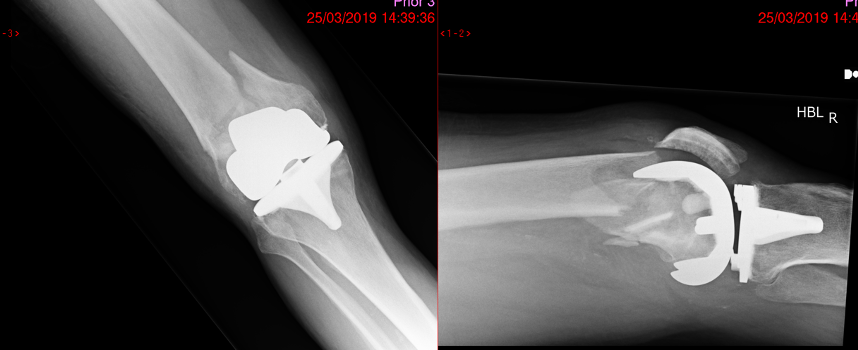
Figure 1.Anteroposterior(AP) and lateral radiographs right knee
Question 1:How: would you describe this injury on the radiographs?
Question 2:What are the likely treatment options you would discuss with patient?
Answer:This is a periprosthetic distal femur fracture around a stable cruciate retaining knee replacement. This can be classified as Type B1 in Unified Classification System (UCS) for periprosthetic fractures. Type B1 and C fractures are usually managed with fixation of the fracture, which can be with a plate or intramedullary nail. Retrograde nailing is a reasonable option when there is adequate distal bone stock to allow a hold with interlocking screws; but this is only possible with cruciate retaining or open box cruciate sacrificing knee replacement. Assessment of the proximal femur and hip is essential for planning the fixation.
Distal femoral replacement is recommended for Type B2 and B3 fractures. This is increasingly popular management option due to the advantage of early mobilisation although this is a complex procedure with associated risks. There are studies looking at the overall cost benefit with a distal femoral replacement due to the less number of days in hospital and earlier return to activity.
The patient was counselled about different treatment options and elected to have fracture fixation with a distal femoral locking plate. She was progressing well at 3 months follow up visit, walking using a single crutch.
Further reading:
Duncan CP, Haddad FS. The Unified Classification System (UCS): improving our understanding of periprosthetic fractures. Bone Joint J. 2014 Jun;96-B (6):713-6.
Darrith B, Bohl DD, Karadsheh MS, Sporer SM, Berger RA, Levine BR Periprosthetic Fractures of the Distal Femur: Is Open Reduction and Internal Fixation or Distal Femoral Replacement Superior?. J Arthroplasty. 2019 Dec 20. pii: S0883-5403(19)31182-9.
She presents 6 months later with sudden increase in pain around the right knee. She has recently increased her activity level with outdoor walking and exercises. Radiographs show breakage of distal screws and secondary displacement of the fracture(Fgure 2).
Question 3:What are the causes of fixation failure?
Question 4:How would you manage the current situation?
Figure 2.Anteroposterior(AP) and lateral radiographs right knee
Answer:The sudden increase in pain around the right knee is due to failure of fracture union leading to fatigue failure of screws. It is important to exclude infection as a cause of fixation failure.This patient subsequently underwent distal femoral replacement after counselling of the various available treatment options(Figure 3 ).
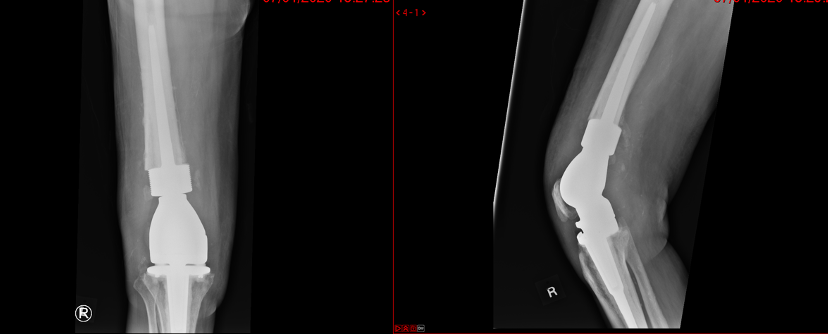
Figure 3.Anteroposterior(AP) and lateral radiographs right knee DFR.
Question: How would you plan to perform the distal femoral replacement for a failed internal fixation?
Answer:This is essentially two operations, metal work removal and distal femoral replacement (DFR)
A high thigh tourniquet may be applied if there is adequate clearance from the surgical field. Surgical approach is the next consideration, as it needs to allow access for removal of plate and screws. It can be performed through a midline knee incision with extension as a lateral subvastus approach or separate lateral incision for removal of plate. The level of bone resection around the distal femur would be dictated by level of fracture, bone quality and available length of prosthesis segment. Restoration of joint line and component rotation can be achieved by marking on the bone before bone resection and trial assessment. In this case, the proximal screws were still intact and taken out with ease. Broken proximal screws are less common but can be an issue as they come in the way of a femoral stem. Intraoperative fluoroscopy is useful to check whether the stem of a DFR has adequately bypassed the screw holes to avoid a stress riser. It is good practice to have adequate bone contact to the hydroxyapatite collar if the DFR prosthesis being used has one. Vigilance for postoperative wound closure and healing is vital as infection and extensor mechanism problems are challenging concerns.
Further reading:
Haidukewych GJ. Role of Distal Femoral Replacement for Periprosthetic Fractures Above a Total Knee Arthroplasty: When and How? J Orthop Trauma. 2019 Sep;33 Suppl 6: S33-S35.